 Understanding Cefazolin Reporting for Enterobacteriaceae
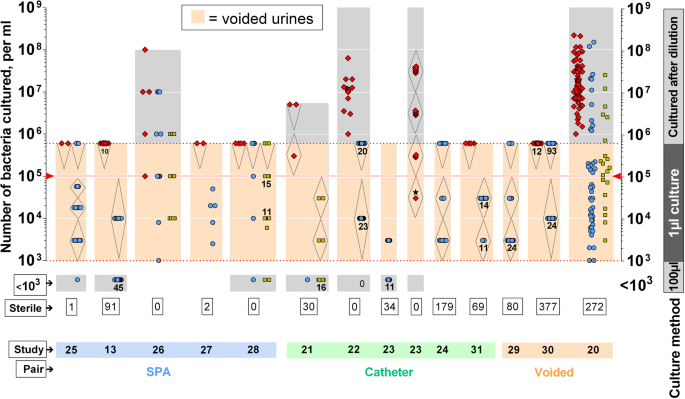
Understanding Cefazolin Reporting for EnterobacteriaceaeNo resultsNo resultsProcessing results.... How is urine culture used in the diagnosis of urinary tract infection (UTI)? The urine culture remains the standard criterion for the diagnosis of UTI. The urine collected must be sent for culture immediately; otherwise, it must be refrigerated at 4°C. Two culture techniques (dip slide, agar) are widely used and accurate. The consensus limits of the Society of Infectious Diseases of America (IDSA) for cystitis and skinonephritis in women are more than 1000 colony formation units (CFU)/mL and more than 10,000 CFU/mL, respectively, for clean average urine specimens. Historically, the definition of UTI was based on the discovery in the culture of 100,000 CFU/mL of a single organism. However, this loses up to 50% of symptomatic infections, so the lower colony rate of more than 1000 CFU/mL is now accepted. [] The definition of asymptomatic bacteriuria still uses the historical threshold. Asymptomatic bacteruria in a female is defined as a culture of urine (white or catheterized specimens) that grows more than 100,000 UF/mL in an asymptomatic individual. Please note that any amount of uropatogen cultivated in the culture of a suprapubic aspiration should be considered evidence of an IU. Approximately 40% of patients with perinepheric abscesses have sterile urine crops. Uncomplicated UTI (cistitis) does not require a culture of urine unless women have experienced a failure of empirical therapy. Get a culture of urine in patients suspected of having a superior UTI or a complicated UTI, as well as those in whom the initial treatment fails. If the patient has had an ITI in the last month, the relapse is probably caused by the same organism. The relapse represents the failure of treatment. Reinfection occurs in 1-6 months and is usually due to a different organism (or serotype of the same organism). Get a urine culture for patients who are reinfected. If a Gram stain of an incentive and clean urine specimen reveals the presence of 1 bacteria per field of oil immersion, it represents 10,000 bacteria/mL of urine. A specimen (5 mL) that has been centrifuged for 5 minutes to 2000 rpm and examined under high power after the Gram stain will identify lower numbers. In general, a Gram stain has a sensitivity of 90% and a specificity of 88%. Related questions:[Guideline] Gupta K, Hooton TM, Naber KG, et al. International clinical practice guides for the treatment of acute cystitis and skinonephritis without complications in women: Update 2010 by the Society of Infectious Diseases of America and the European Society of Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar. 52(5):e103-20. . .[Guideline] Wagenlehner FM, Schmiemann G, Hoyme U, Fünfstück R, Hummers-Pradier E, Kaase M, et al. [National guide S3 on infection of the urinary tract without complications: recommendations for the treatment and management of bacterial infections of the urinary tract without complications acquired by the community in adult patients]. Urologe A. 2011 Feb. 50(2):153-69. Abrahamian FM, Moran GJ, Talan DA. Urinary tract infections in the emergency department. Infect Dis Clin North Am. 2008 Mar. 22(1):73-87, vi. . Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al. Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomized trial, economic analysis, observational cohort and qualitative study. Health Technol Assess. 2009 Mar. 13(19):iii-iv, ix-xi, 1-73. Lane DR, Takhar SS. Diagnosis and management of urinary tract infection and skinonephritis. Emerg Med Clin North Am. 2011 Aug. 29(3):539-52. . Czaja CA, Stamm WE, Stapleton AE, et al. Prospective study of cohorts of microbial and inflammatory events immediately before Escherichia coli recurrent infection of the urinary tract in women. J Infect Dis. 2009 Aug 15. 200(4):528-36. Adeghate J, Juhász E, Pongrácz J, Rimanóczy É, Kristóf K. Does Staphylococcus Saprophyticus cause acute cystitis only in young females, or is there more in history? A one-year comprehensive study in Budapest, Hungary. Acta Microbiol Immunol Hung. 2016 Mar. 63 (1):57-67. Kanj SS, Kanafani ZA. Current concepts in antimicrobial therapy against resistant gram-negative organisms: beta-lactamase-production of Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and Pseudomonas aeruginosa multirresistent. May Clin Proc. 2011 Mar. 86(3):250-9. . .[Guideline] Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention and treatment of urinary tract infection associated with adult catheter: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010 Mar 1. 50(5):625-63. . . Tiemstra JD, PD Boy, Pela E. Genitourinary infections after a routine pelvic exam. J Am Board Fam Med. 2011 May-Jun. 24(3):296-303. Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Outpatient Health Care Survey: Summary of 2007. Natl Health Stat Report. 2010 Nov 3. 1-32. . Naber KG, Schito G, Botto H, Palou J, Mazzei T. Surveillance study in Europe and Brazil on clinical aspects and Epidemiology of Antimicrobial Resistance in Women with Cistitis (ARESC): implications for empirical therapy. Eur Urol. 2008 Nov. 54(5):1164-75. . Little P, Merriman R, Turner S, Rumsby K, Warner G, Lowes JA, et al. Presentation, pattern and natural course of severe symptoms, and the role of antibiotics and antibiotic resistance among patients who have suspected urinary tract infection not complicated in primary care: observational study. BMJ. 2010 Feb 5. 340:b5633. . . Molander U, Arvidsson L, Milsom I, Sandberg T. Longitudinal cohort study of older women with urinary tract infections. Maturitas. 2000 Feb 15. 34(2):127-31. Johnson L, Sabel A, Burman WJ, Everhart RM, Rome M, MacKenzie TD, et al. Fluoroquinolone resistance emergency in urinary insulations of Escherichia coli ambulatory. Am J Med. 2008 Oct. 121(10):876-84. . [Guideline] American College of Obstetricians and Gynecologists (ACOG). 2008. Treatment of urinary tract infections in non-pregnant women. Available in . Access: September 22, 2010. Barclay L. Urinary Tract Infection: 3 Diagnostic Questions for Women's Aid. Medscape Medical News. Available in . Access: September 16, 2013. Knottnerus BJ, Geerlings SE, Moll van Charante EP, Ter Riet G. Towards a simple diagnostic index for acute urinary tract infections without complications. Ann Fam Med. 2013 Sep-Oct. 11(5):442-51. Schaeffer AJ, Schaeffer EM. Urinary Tract infections. In: McDougal WS, Wein AJ, Kavoussi LR, et al, eds. Campbell-Walsh Urology. 10th Ed. Philadelphia, PA: Elsevier Saunders; 2012. 46-55. Lifshitz E, Kramer L. External urine culture: Does the collection technique matter? Arch Intern Med. 2000 Sep 11. 160(16):2537-40. Propp DA, Weber D, Ciesla ML. Fiability of a urine dipstick in patients in the emergency department. Ann Emerg Med. 1989 May. 18(5):560-3. Mehnert-Kay SA. Diagnosis and Management of Uncomplicated Urinary Infections. American Family Physician. August 1, 2005. 27/No.3:1-9. .[Guideline] Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guidelines for the prevention of urinary tract infections associated with catheter 2009. Infect Control Hosp Epidemiol. 2010 Apr 31(4):319-26. Kauffman CA, Fisher JF, Sobel JD, Newman CA. Candidate urinary tract infections: diagnosis. Clin Infect Dis. 2011 May. 52 Suppl 6:S452-6. . Falagas ME, Kotsantis IK, Vouloumanou EK, Rafailidis PI. Antibiotics against placebo in the treatment of women with uncomplicated cystitis: a randomized controlled metaanalysis. J Infect. 2009 Feb. 58(2):91-102. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010 Dec. 7(12):653-60. . Little P, Moore MV, Turner S, Rumsby K, Warner G, Lowes JA, et al. Effectiveness of five different approaches in managing urinary tract infection: randomized controlled trial. BMJ. 2010 Feb 5. 340:c199. . .Lavigne JP, Bruyère F, Bernard L, Combescure C, Ronco E, Lanotte P, et al. Power of resistance and virulence of uropatogenic strains Escherichia coli isolated from patients hospitalized in urology departments: a prospective French multicenter study. J Med Microbiol. 2016 Jun. 65 (6):530-7. . Christiaens TC, De Meyere M, Verschraegen G, Peersman W, Heytens S, De Maeseneer JM. Randomized nitrofurantoin controlled trial against placebo in the treatment of urinary tract infection without complications in adult women. Br J Gen Pract. 2002 Sep. 52(482):729-34. . .Bleidorn J, Gágyor I, Kochen MM, Wegscheider K, Hummers-Pradier E. Symptomatic treatment (ibuprofen) or antibiotics (ciprofloxacin) for urinary tract infection without complications? - results of a randomized controlled pilot trial. BMC Med. 2010 May 26. 8:30. . .Grigoryan L, Zoorob R, Wang H, Trautner BW. Low book With Guidelines for Treatment of Acute Cystitis in Primary Care. Open Forum Infect Dis. 2015 Dec. 2 (4):ofv159. Sigler M, Leal JE, Bliven K, Cogdill B, Thompson A. Assessment of appropriate antibiotic prescribing for urinary tract infection in an internal medicine clinic. South Med J. 2015 May. 108 (5):300-4. . Olson RP, Harrell LJ, Kaye KS. Antibiotic resistance in urinary insulations of Escherichia coli of female university students with urinary tract infections. Antimicrob Agents Chemother. 2009 Mar. 53(3):1285-6. McKinnell JA, Stollenwerk NS, Jung CW, Miller LG. Nitrofurantoin favorably compares with recommended agents as empirical treatment of urinary tract infections not complicated in a decision and cost analysis. May Clin Proc. 2011 Jun. 86(6):480-8. . .Falagas ME, Vouloumanou EK, Togias AG, Karadima M, Kapaskelis AM, Rafailidis PI, et al. Fosfomycin versus other antibiotics for the treatment of cystitis: a randomized controlled meta-analysis. J Antimicrob Chemother. 2010 Sep. 65(9):1862-77. . .[Guideline] Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases The American Society guides the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005 Mar 1. 40(5):643-54. Dalalal S, Nicolle L, Marrs CF, Zhang L, Harding G, Foxman B. The asymptomatic bacteria of Escherichia coli among women with diabetes mellitus. Clin Infect Dis. 2009 Aug 15. 49(4):491-7. . .Beerepoot MA, ter Riet G, Nys S, et al. Cranberries vs antibiotics to prevent urinary tract infections: a randomized trial of non-double blind inferiority in premenopausal women. Arch Intern Med. 2011 Jul 25. 171(14):1270-8. Jepson RG, Craig JC. Kangaroo to prevent urinary tract infections. Cochrane Database Syst Rev. 2008 Jan 23. CD001321. . Tempera G, Corsello S, Genovese C, Caruso FE, Nicolosi D. Inhibitive activity of the cranberry extract on bacterial adhesiveness in the urine of women: an ex-living study. Int J Immunopathol Pharmacol. 2010 Abr-Jun. 23(2):611-8. . Frellick M. Drinking more water reduces repeated urinary tract infections. Medscape Medical News. Available in . October 9, 2017; Access: October 10, 2017. De Vita D, Giordano S. Intravesical hyaluronic acid/condroitin sulphate in recurrent bacterial cystitis: a randomized study. Int Urogynecol J. 2012 Dec. 23(12):1707-13. Anger J, Lee U, Ackerman AL, Chou R, Chughtai B, Clemens JQ, et al. Recurrent infections of the urinary tradition in women: AUA/CUA/SUFU Guion. J Urol. 2019 May 1. 101097JU0000000296. .van der Starre WE, van Nieuwkoop C, Paltansing S, et al. Risk Factors for Fluoroquinolone-resistant Escherichia coli in adults with urinary infection of febriles as a whole. J Antimicrob Chemother. 2011 Mar. 66(3):650-6. . Cloutier DJ, Miller LG, Komirenko AS, Cebrik DS, Krause KM, Keepers TR, et al. Plazomicin Versus Meropenem for the treatment of complicated urinary infection and acute skinonephritis: Results of the EPIC study. Presented at the 27th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Vienna, Austria, 22-25 April 2017. Cunha BA. Prophylaxis for recurrent urinary tract infections: nitrofurantoin, not trimethoprim-sulfamethoxazole or cranberry juice. Arch Intern Med. 2012 Jan 9. 172(1):82; author 82-3 response. Cunha BA, Schoch PE, Hage JR. Nitrofurantoin: Preferred empirical therapy for lower urinary tract infections acquired by the community. May Clin Proc. 2011 Dec. 86(12):1243-4; author's reply 1244. .Fischer HD, Juurlink DN, Mamdani MM, Kopp A, Laupacis A. Hemorragia during warfarin therapy associated with cotrimoxazole and other anti-infective agents of the urinary tract: a population-based study. Arch Intern Med. 2010 Apr 12. 170(7):617-21. . L.: Reporting offers long-needed clarity. Medscape [serial online]. Available in . Access: 18 November 2013. Hooton TM, Roberts PL, Cox ME, Stapleton AE. Average-current urine and acute cystitis in premenopausal women. N Engl J Med. 2013 Nov 14. 369(20):1883-91. . Leydon GM, Turner S, Smith H, Little P. Women's views about management and cause of urinary tract infection: qualitative interview study. BMJ. 2010 Feb 5. 340:c279. Pinson AG, Philbrick JT, Lindbeck GH, Schorling JB. Acute skin management in women: a cohort study. Am J Emerg Med. 1994 May. 12(3):271-8. . Turner D, Little P, Raftery J, Turner S, Smith H, Rumsby K, et al. Cost effectiveness of management strategies for urinary tract infections: results of randomized controlled trial. BMJ. 2010 Feb 5. 340:c346. . . John L Brusch, MD, Assistant Professor of Medicine at FACP, Harvard Medical School; Consulting Cabinet, Department of Medicine and Infectious Diseases, Cambridge Health Alliance John L Brusch, MD, FACP is a member of the following medical societies: , Disclosure: Nothing to reveal. Mary F Bavaro, MD Fellowship Director, Division of Infectious Diseases, Navy Medical Center, San Diego Mary F Bavaro, MD is a member of the following medical societies: , Disclosure: Nothing to reveal. Burke A Cunha, MD Professor of Medicine, State University of New York School of Medicine at Stony Brook; Chief, Infectious Disease Division, Winthrop-University Hospital Burke A Cunha, MD is a member of the following medical societies: , , Disclosure: Nothing to reveal. Jeffrey M Tessier, MD Associate Professor, Division of Infectious Diseases, Department of Internal Medicine, University of Virginia Medical School Jeffrey M Tessier, MD is a member of the following medical societies: Disclosure: Nothing to reveal. Michael Stuart Bronze, MD David Ross Boyd Professor and President of the Department of Medicine, Stewart G Wolf Doted President in Internal Medicine, Department of Medicine, University of Oklahoma Health Science Center; Master of the American College of Physicians; Fellow, Infectious Diseases Society of America; Fellow of the Royal College of Physicians, London Michael Stuart Bronze, MD is a member of the following medical societies: , , , , , , , Disclosure: Nothing to reveal. Michael S Beeson, MD, MBA, FACEP Emergency Medicine Professor, Northeastern Ohio University College of Medicine and Pharmacy; Attending Faculty, Akron General Medical CenterMichael S Beeson, MD, MBA, FACEP is a member of the following medical societies: , , , , and Disclosure: Nothing to reveal. Pamela L Dyne, Professor of Clinical Medicine/Emergency Medicine, University of California, Los Angeles, David Geffen School of Medicine; Attending Physician, Department of Emergency Medicine, Olive View-UCLA Medical Center Pamela L Dyne, MD is a member of the following medical societies: , , and Divulgation: Nothing to reveal. David S Howes, Professor of Medicine and Pediatrics at the University of Chicago, Director of the Medical Residence Program of the Section and Emergency Medicine, Division of Biological Sciences of the University of Chicago, Pritzker School of Medicine David S Howes, MD is a member of the following medical societies: , , and Divulgation: Nothing to reveal. Elicia S Kennedy, MD Clinical Assistant Professor, Department of Emergency Medicine, University of Arkansas for Medical Sciences Elicia S Kennedy, MD is a member of the following medical societies: American College of Emergency Physicians and Society for Academic Emergency Medicine Disclosure: Nothing to reveal. Klaus-Dieter Lessnau, MD, FCCP Associate Professor of Clinical Medicine, Faculty of Medicine of the University of New York; Medical Director, Laboratory of Physiology Pulmonary; Director of Research in Medicine Pulmonary, Department of Medicine, Section of Medicine Pulmonary, Hospital Lenox Hill Klaus-Dieter Lessnau, MD, FCCP is a member of the following medical societies: Mark Jeffrey Noble, MD Consulting Staff, Urologic Institute, Cleveland Clinic Foundation Mark Jeffrey Noble, MD is a member of the following medical societies: , , , , , , Society of University Urologists and Dissemination: Nothing to reveal. Adam J Rosh, MD Assistant Professor, Department of Emergency Medicine, Detroit Reception Hospital, Wayne State University School of MedicineAdam J Rosh, MD is a member of the following medical societies: , , and disclosure: Nothing to reveal. Joseph A Salomone III, MD Associate Professor and Attending Staff, Truman Medical Centers, University of Missouri-Kansas City School of Medicine; EMS Medical Director, Kansas City, MissouriJoseph A Salomone III, MD is a member of the following medical societies: , , and disclosure: Nothing to reveal. Richard H Sinert, DO Associate Professor of Emergency Medicine, Assistant Professor of Medicine, Director of Research, New York State University School of Medicine; Consulting Cabinet, Department of Emergency Medicine, Hospital Center of KingsRichard H Sinert County, DO is a member of the following medical societies: and Disclosure: Nothing to reveal. Francisco Talavera, PharmD, PhD Associate Professor, University of Nebraska Medical Center College of Pharmacy; Chief Editor, Medscape Drug ReferenceDisclosure: Medscape Salary Employment Mark Zwanger, MD, Associate Professor of MBA, Department of Emergency Medicine, Medical Jefferson College of Thomas Jefferson University Mark Zwanger, MD, MBA is a member of the following medical societies: , , and Disclosure: Nothing to reveal: Find About UsAboutMembershipWebMD NetworkEditions
Main menu User menuSearchAccess Denied You are not authorized to access this page "news/aapnewsmag/2017/03/27/IDSnapshot032717.full.pdf". Individual access Log in You can get access using your login credentials for your institution. Contact your librarian or administrator if you do not have a username and password. Enter through your institution Access to purchase

Interpretation of urine cultures
Interpretation of urine cultures
Urinary Tract Infections in Adults - American Family Physician
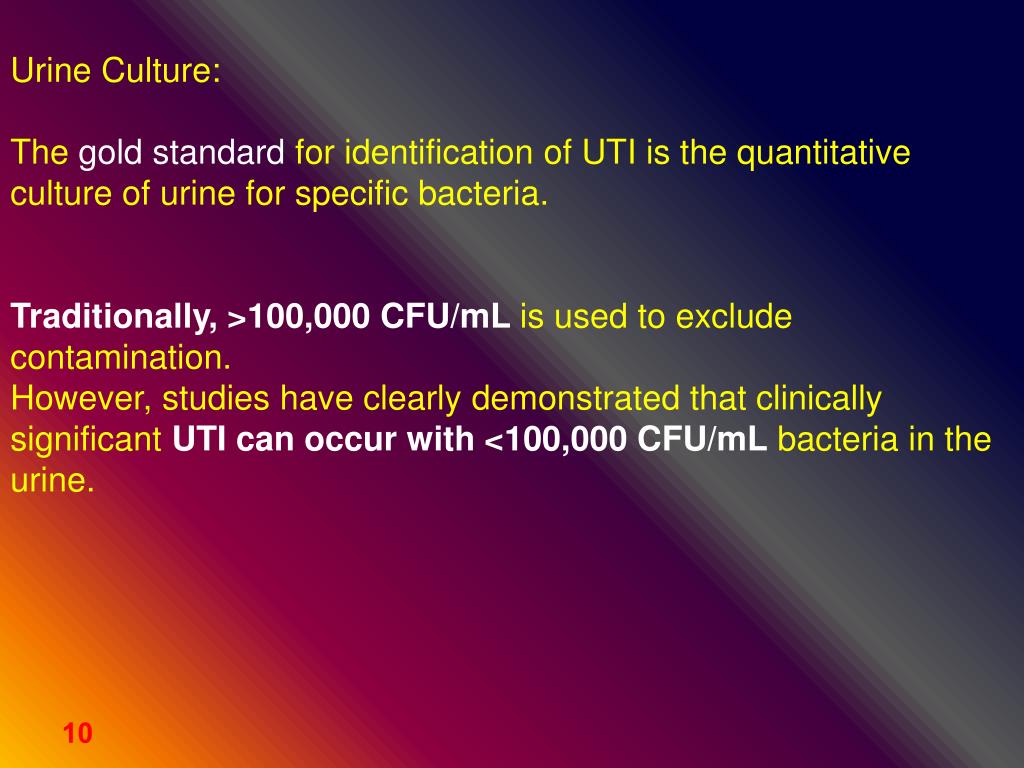
Urine culture. - ppt download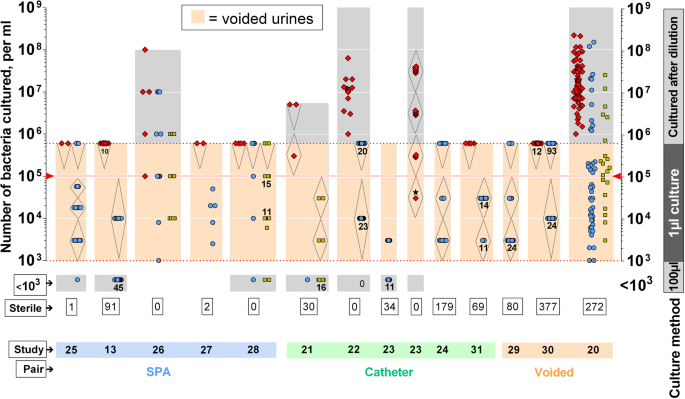
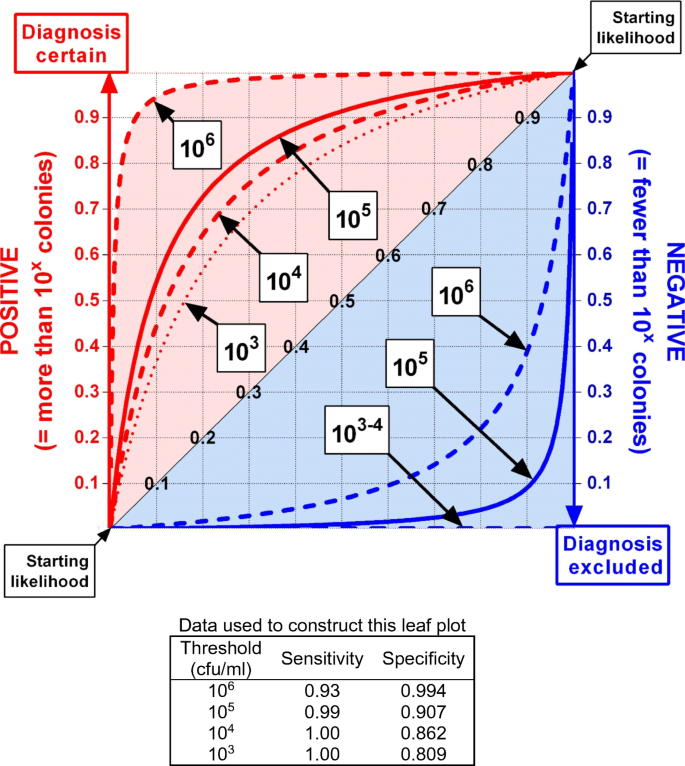
Defining urinary tract infection by bacterial colony counts: a case for 100,000 colonies/ml as the best threshold | SpringerLink
VetBact
Urinary Tract Infection | Encyclopedia
E. coli and Urinary Tract Infections (UTIs) | Everyday Health
E. coli resistant to colistin and carbapenems foundin U.S. patient | PM360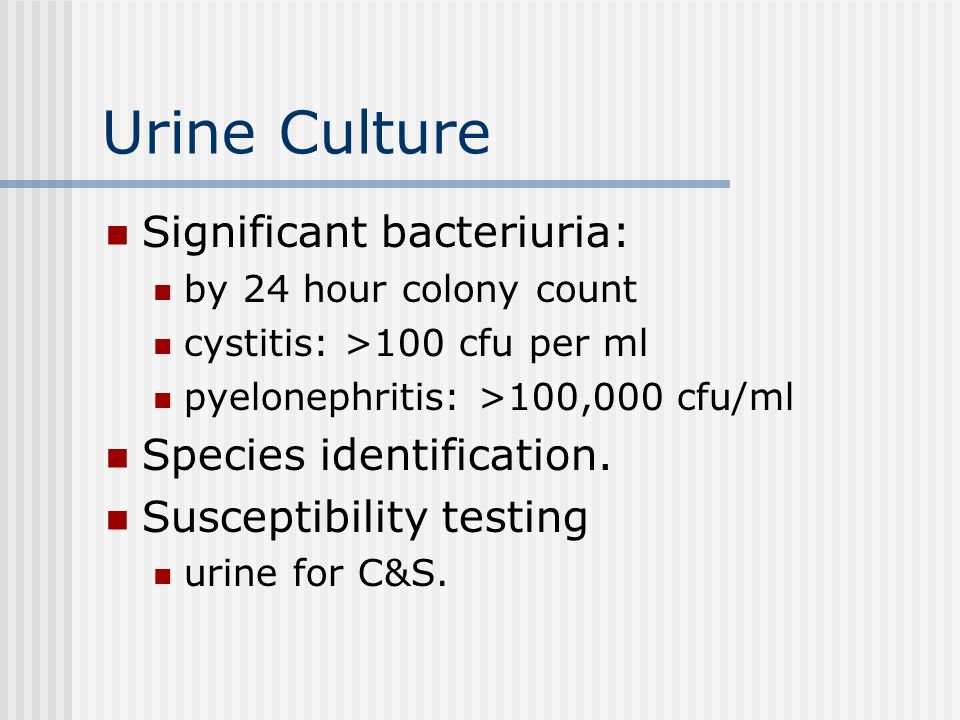
UTIs-Definition Infectious diseases of the urinary tract: - ppt video online download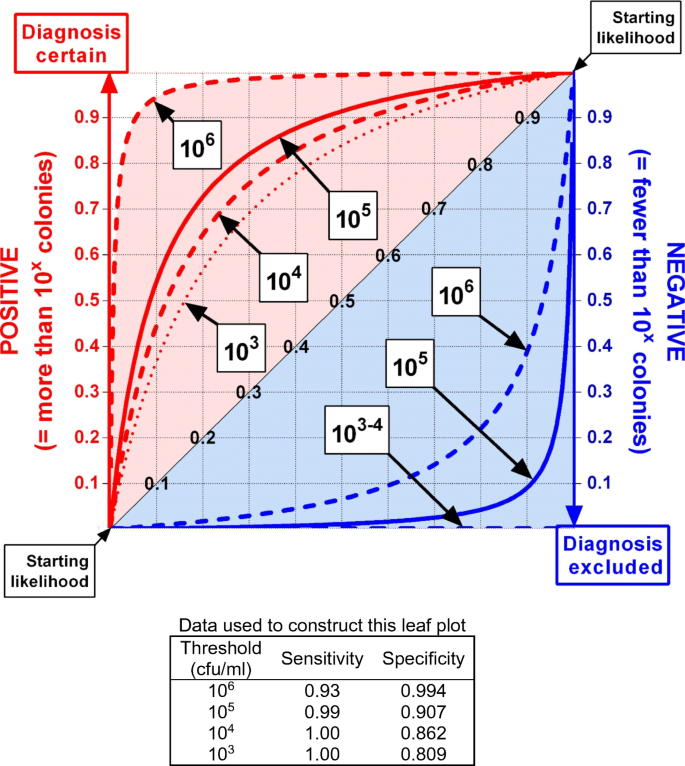
Defining urinary tract infection by bacterial colony counts: a case for 100,000 colonies/ml as the best threshold | SpringerLink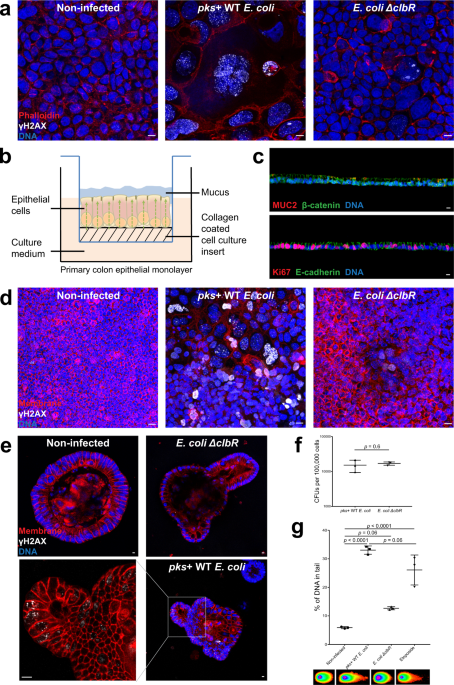
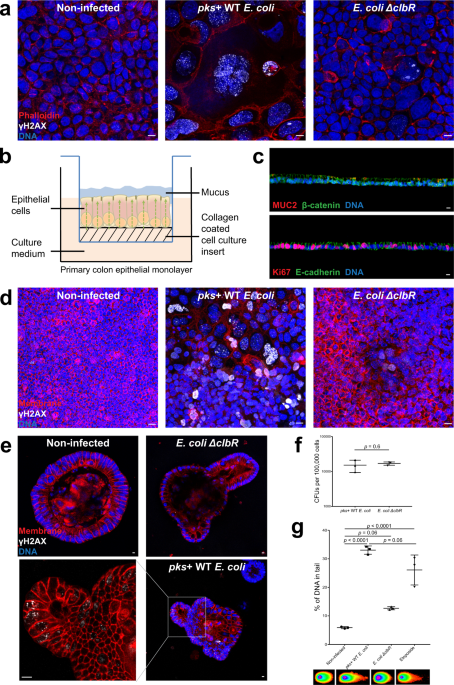
Genomic aberrations after short-term exposure to colibactin-producing E. coli transform primary colon epithelial cells | Nature Communications
URINARY TRACT INFECTION - ppt video online download
BACTERIAL INFECTIONS - Urinalysis and Body Fluids
Escherichia Coli Grown> 100000 Cfu/ml - Hi, Few Days Back | Practo Consult
Urinary tract infections – Introduction, clinical features and diagnosis Dr. - ppt video online download
Rapid Detection of Urinary Tract Infections via Bacterial Nuclease Activity: Molecular Therapy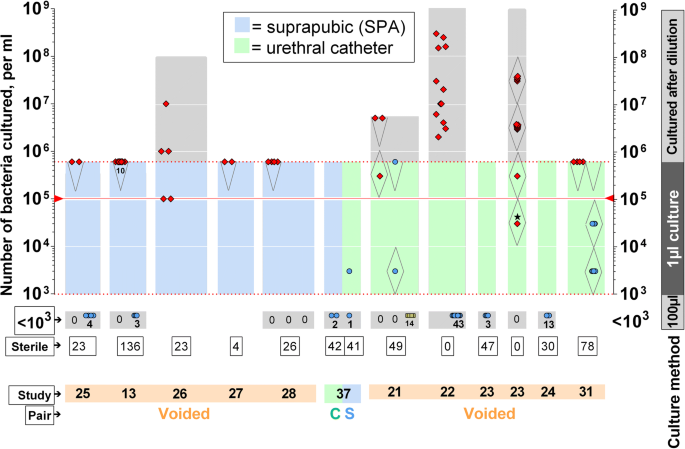
Defining urinary tract infection by bacterial colony counts: a case for 100,000 colonies/ml as the best threshold | SpringerLink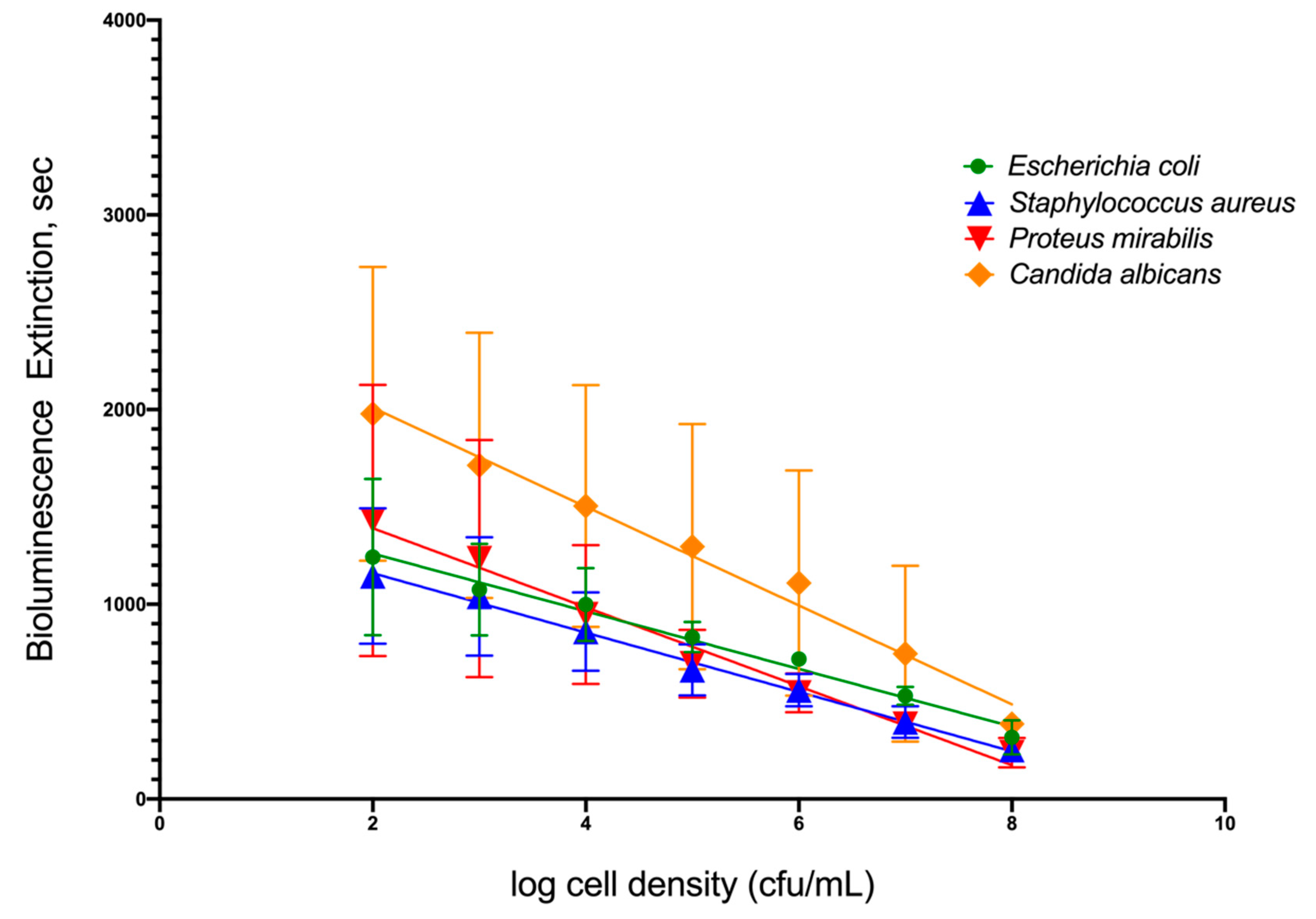
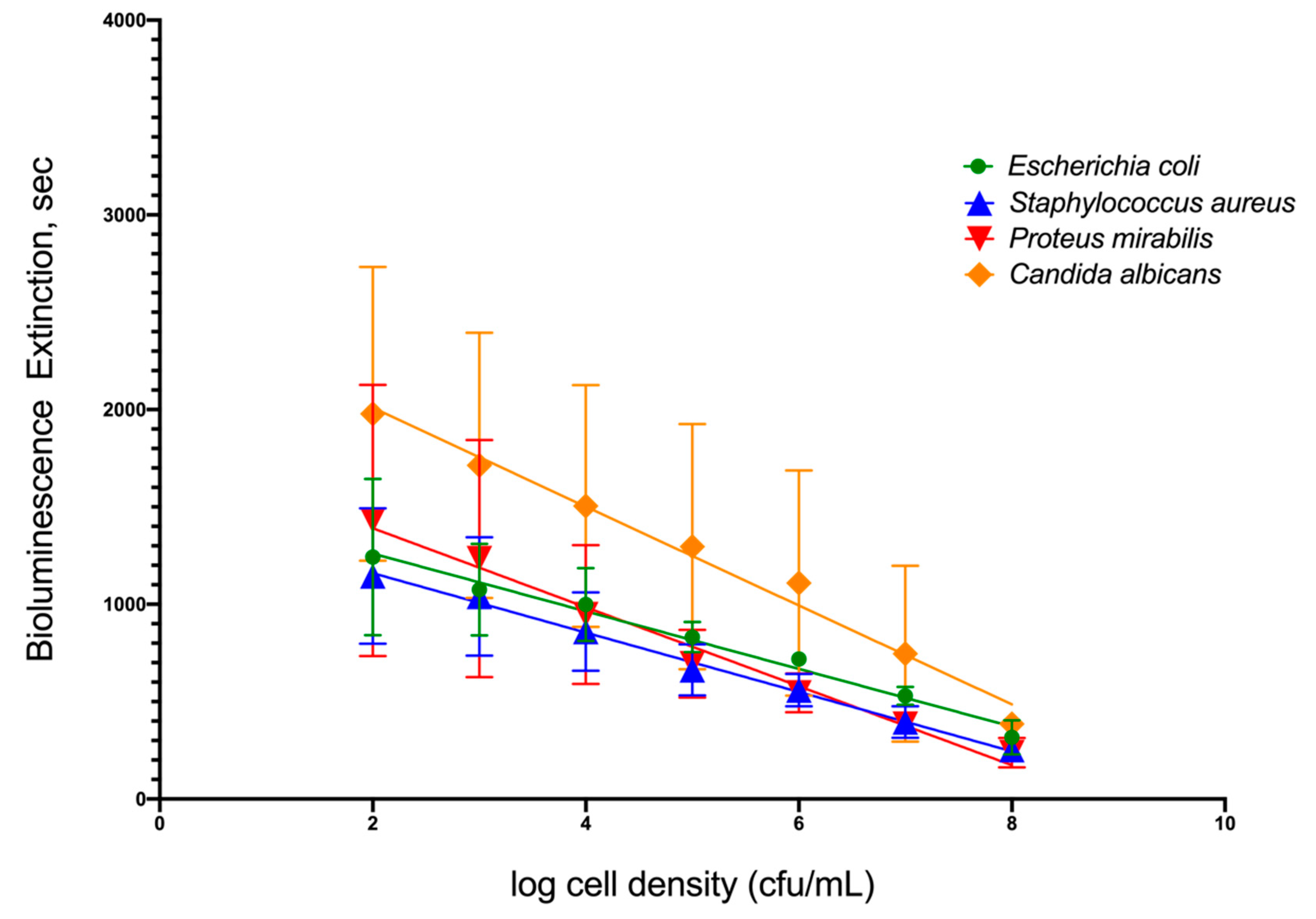
IJMS | Free Full-Text | An Intact Cell Bioluminescence-Based Assay for the Simple and Rapid Diagnosis of Urinary Tract Infection | HTML
Sensitivity of RAPD-HRM for E. coli detection (a) CFU assay coordinated... | Download Scientific Diagram
Gold Nanorod Based Selective Identification of Escherichia coli Bacteria Using Two-Photon Rayleigh Scattering Spectroscopy. - Abstract - Europe PMC
My baby is 70 days old. Urine culture report was clonov count > 100000 /ml. Doctor gave cephalexin syrup. In repeat culture also got the same result. Few epithelial cells, pus cells
Diagnosis and imaging of neonatal UTIs - Pediatrics & Neonatology
Study of the risk factors related to acquisition of urinary tract infections in patients submitted to renal transplant
Interpretation of urine cultures
Molecular Diagnosis of Urinary Tract Infections by Semi-Quantitative Detection of Uropathogens in a Routine Clinical Hospital Setting. - Abstract - Europe PMC
PDF) Risk factors for bacteriuria due to Pseudomonas aeruginosa or Enterococcus spp in patients hospitalized via the emergency department
E. coli Video - YouTube
Profile of antimicrobial resistance of bacteria isolated from cockroaches (Periplaneta americana) in a Brazilian health care institution
IJMS | Free Full-Text | An Intact Cell Bioluminescence-Based Assay for the Simple and Rapid Diagnosis of Urinary Tract Infection | HTML
Rapid Detection of Urinary Tract Infections via Bacterial Nuclease Activity: Molecular Therapy
Urinary Tract Infections | The Hsieh Lab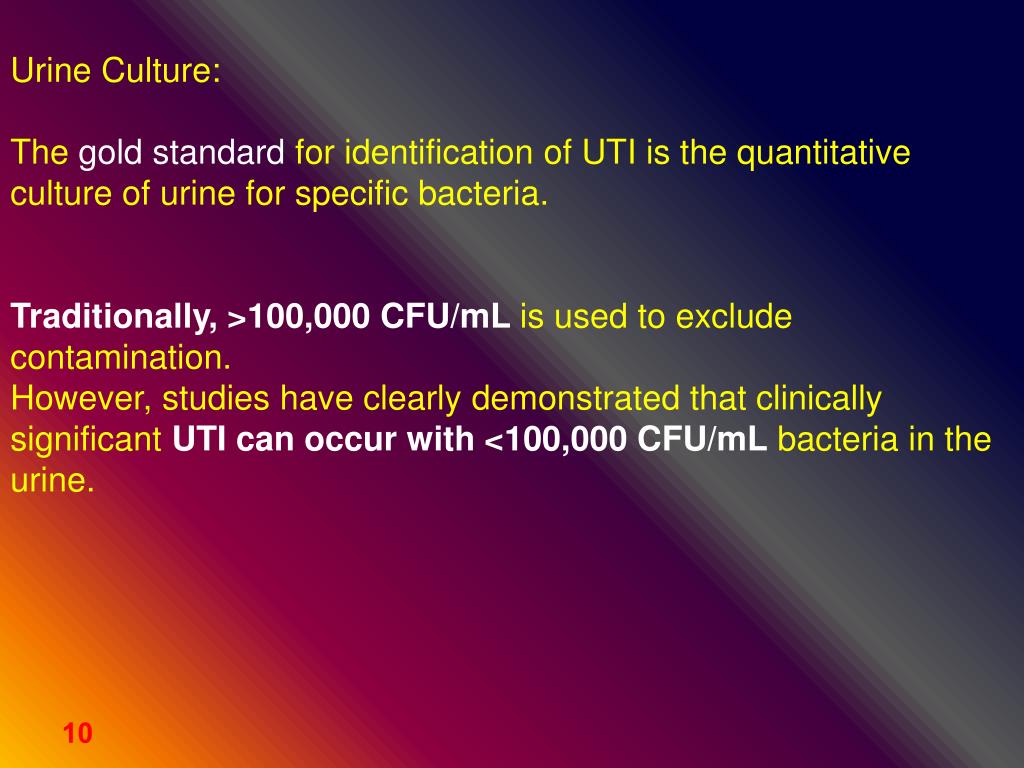
PPT - URINARY TRACT INFECTION PowerPoint Presentation, free download - ID:4951462
WO2015187638A2 - Method of reducing e. coli or salmonella contamination of agricultural products - Google Patents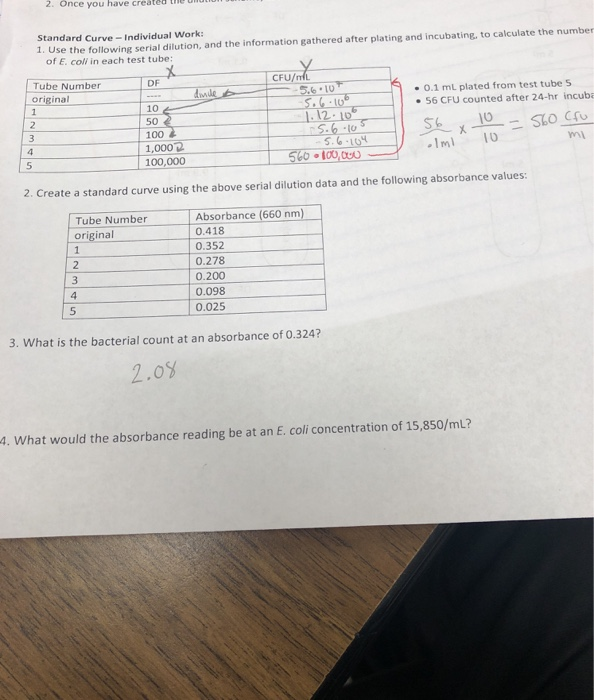
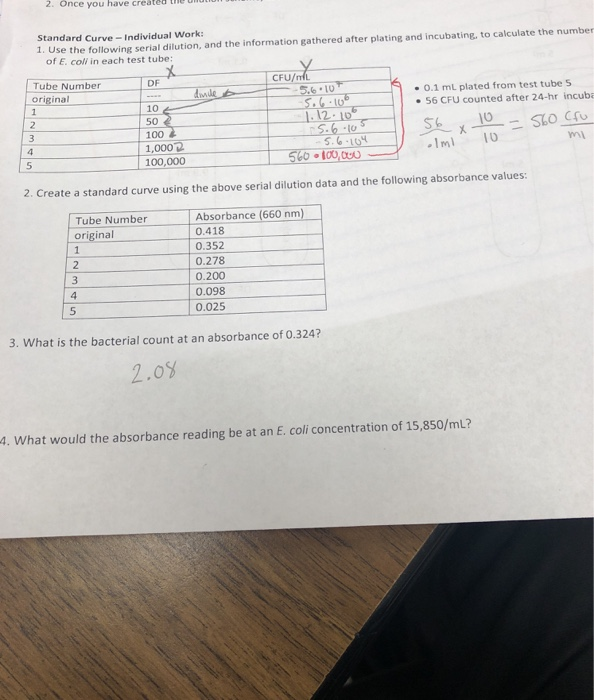
Solved: 2. Once You Have Created Th Standard Curve - Indiv... | Chegg.com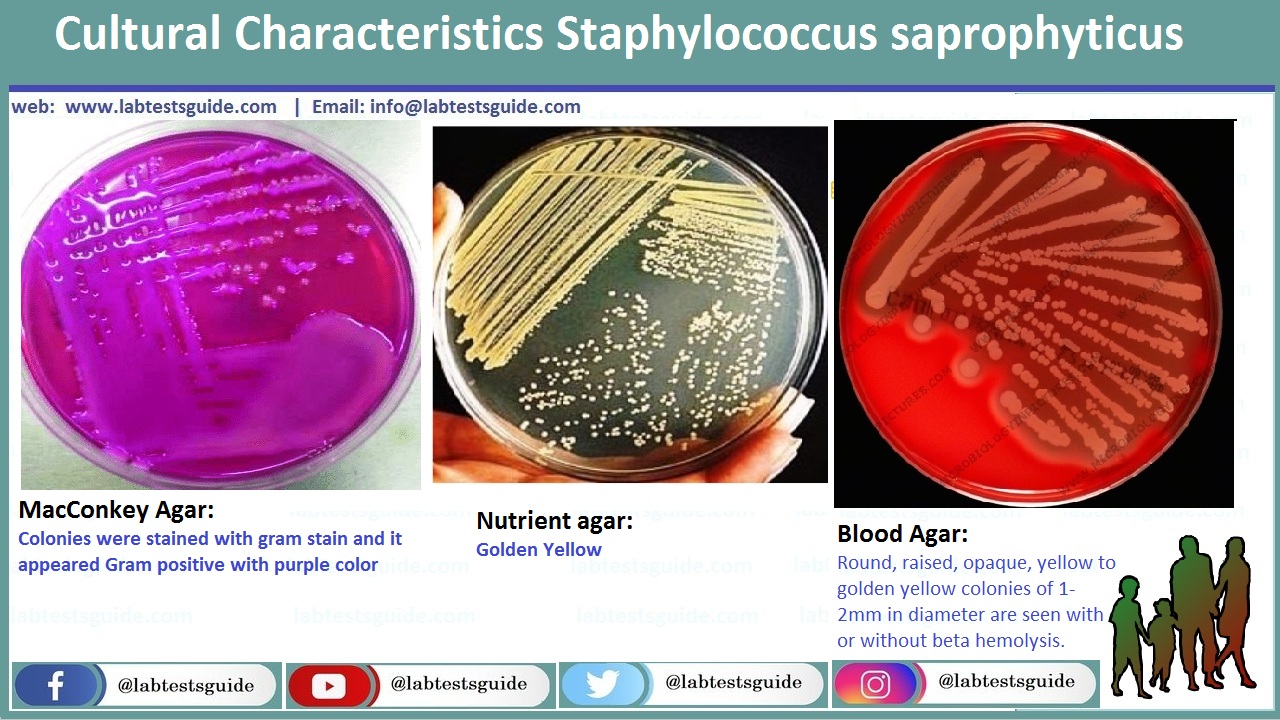
Urine Culture Interpretation, Identification and more | Lab Tests Guide
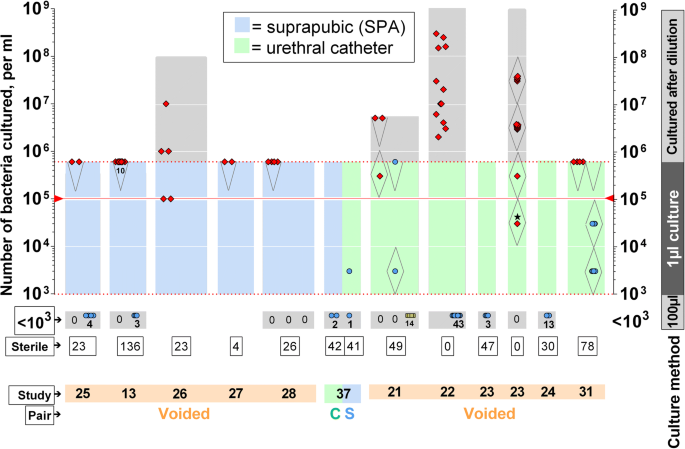
The Clinical Urine Culture: Enhanced Techniques Improve Detection of Clinically Relevant Microorganisms. - Abstract - Europe PMC
Urinary tract infections – Introduction, clinical features and diagnosis Dr. - ppt video online download
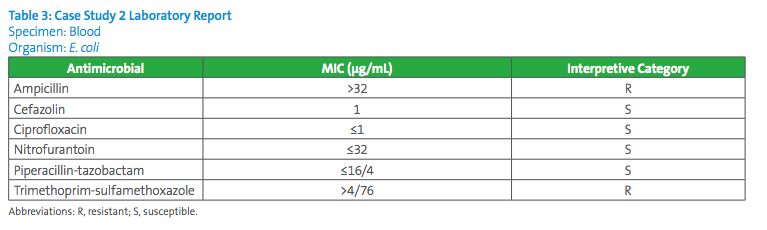
CAUTI Case Studies Functional Exercises Louisiana NHSN Trainings 2017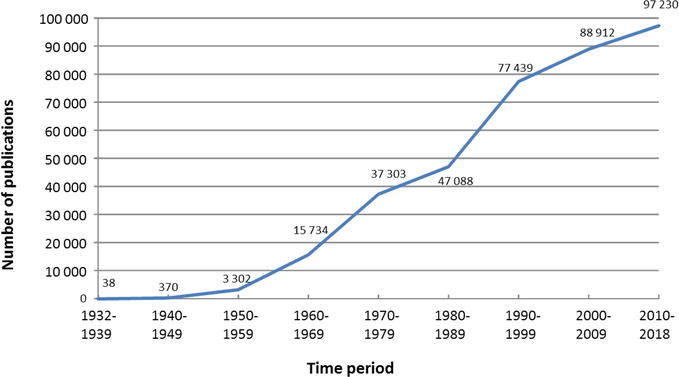
Introductory Chapter: The Versatile Escherichia coli | IntechOpen
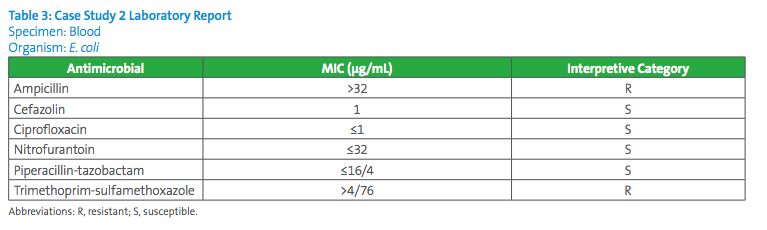 Understanding Cefazolin Reporting for Enterobacteriaceae
Understanding Cefazolin Reporting for Enterobacteriaceae






















Posting Komentar untuk "100000 cfu ml escherichia coli"